Top > About Us > News Letter > To provide cutting-edge treatment for rectal cancer
To provide cutting-edge treatment for rectal cancer
A message from the University of Tokyo Hospital to the world
Colon and Rectal Surgery
Soichiro Ishihara, Professor and Chairman
1: Colorectal cancer and rectal cancer
The incidence of colorectal cancer has been gradually increasing in Japan as a result of the westernization of lifestyle. Recent statistics show that colorectal cancer is second only to lung cancer as the leading cause of cancer-related deaths. Fortunately, the prognosis for colorectal cancer is relatively good and it is said that, if appropriate treatment is provided, about 70% of patients can be saved. Care after recovering from cancer is therefore also important. In addition to selecting the optimal treatment for each patient, considerable emphasis should be placed on preventing the deterioration of quality of life due to treatment as much as possible. Cancer developing in the rectum, which is the part of the large intestine closest to the anus, has clinical features and problems different from those of other colorectal cancers as follows:
-Difficult to operate on due to the narrowness of the space, surrounded as it is by the pelvis
-The prostate, bladder and other important organs near the rectum need to be preserved appropriately.
-The nerves distributed around the bladder and prostate, which run in the vicinity of the rectum, can be unintentionally cut during surgery, sometimes resulting in deterioration of sexual and urinary functions after surgery.
-Even if cancer macroscopically seems to have been completely removed, minute cancers may remain unremoved, which can cause a relapse. (This is called local recurrence.)
-Depending on the location of the cancer, in some cases even the anus must be resected, which may result in a permanent stoma.
In an attempt to overcome these problems, our department has been actively applying preoperative chemoradiotherapy (CRT) and robotic surgery.
2: Preoperative chemoradiotherapy (CRT)
When a rectal cancer is detected, instead of immediately proceeding to surgery, treatment starts with a combination of anticancer drugs and radiation for about one and a half months. After completing the combination therapy, we wait for about two months until the cancer becomes small enough to be surgically removed (Figure 1). The more the cancer shrinks, the smaller the resection area. If you treat tumor cells that are too small to be seen in advance of surgery, the risk of local recurrence following surgery can be reduced. This treatment method has been adopted for years in Europe and the United States, but has not prevailed in clinical practice in Japan. Our department started employing radiation therapy in 1985, earlier than any other hospital in Japan, and, since 2003, has performed chemoradiotherapy (CRT), a combination of radiotherapy and anticancer drugs. More than 400 patients have so far received this treatment at our hospital. The Guidelines for the Treatment of Colorectal Cancer, revised this year, recommend that preoperative CRT be performed for rectal cancer with a high risk of local recurrence.
We also take measures to further enhance the effect of CRT. Among patients showing a very good response to CRT, there are some whose cancer is completely eradicated (complete response) only with CRT. With conventional methods alone, however, complete response was achieved only in about 10% of those undergoing therapy. We therefore additionally use an anticancer agent, irinotecan, to enhance the therapeutic effect. As a result, we successfully raised the ratio of complete response to nearly 20%. In parallel with this effort, the hospital’s affiliated laboratory has been engaged in basic research related to radiotherapy to search for methods to further enhance the therapeutic effects.
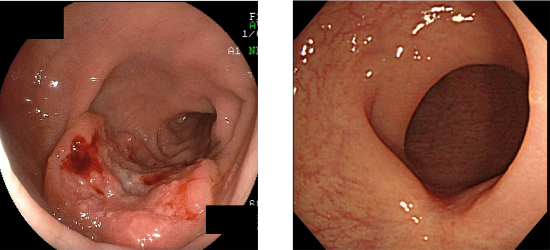
Figure 1: Before and after chemoradiotherapy (CRT)
Rectal cancer before treatment (left); Rectal cancer in the same patient after CRT (Hardly any tumors remain.) (right)
3: Minimally invasive surgery and robotic surgery
In the last ten years or so, laparoscopic, robotic and other minimally invasive surgeries have rapidly become widely used to treat colorectal cancer. At our hospital, minimally invasive surgeries account for more than 90% of colorectal cancer surgeries. In these surgeries, we frequently use a surgical robot called da Vinci to treat rectal cancer (Figure 2). The rectum is located in a narrow area surrounded by the hard, bony pelvis. If a large rectal cancer is located in this area, linear surgical tools cannot reach the other side of the cancer, sometimes making it difficult to treat. The da Vinci surgical system has seven joints on each arm. These joints allow the surgeon’s hand movements on the control board to be accurately transmitted to the tip of the arm in the peritoneal cavity. The surgeon can manipulate the system’s arms to perform the surgery as if his/her own hands were inside the peritoneal cavity. The system is designed in such a way that the tips can flexibly bend in the narrow area in the pelvis to ensure a precise resection. It also allows the structure of fine nerves to be visualized in detail, three-dimensionally. It is expected that this function of the system helps preserve nerves distributed in the prostate and bladder without damaging them, and thus prevents sexual and urinary functions from deteriorating after surgery. Our hospital has used robotic surgery for rectal cancer since 2012 and nearly 200 patients have undergone the surgery. At the beginning, the cost for robotic surgery, which was more than two million yen, was not covered by health insurance. This high cost had been a hindrance until April last year when health insurance coverage was approved. At present, patients can receive robotic surgery at a cost not much different from that of ordinary laparoscopic surgery.

Figure 2: Robotic surgery