Top > About Us > News Letter > Pneumonia in elderly people
Pneumonia in elderly people
Routine vaccination against pneumococcus for elderly people started last October.
We asked Dr. Yasuhiro Yamaguchi, Lecturer in the Department of Geriatric Medicine, about pneumonia in elderly people and its prevention.
Easy to become severe in elderly people
Pneumonia in elderly people can easily become severe compared to that in younger people and its life-threatening rate is significantly high. Although young people rarely die of pneumonia, mortality starts to increase at more than 65 years old, and at 85 years old or older, it becomes more than 1,000 times higher than that in younger people. Because of the increasing number of elderly people, pneumonia recently became the third leading cause of death of Japanese people, behind malignant tumors and cardiac diseases.
Frequently observed pneumonia in elderly people and its cause
There is more than one cause of pneumonia. The most frequently observed pneumonia in elderly people is aspiration pneumonia. It occurs when food gets into the airway that is connected to the lung, instead of getting into the esophagus (because the ability to swallow becomes weaker) or when secretions or bacteria in the mouth or a tiny amount of regurgitated digestive fluid get into the lung. Pneumonia after viral infections, such as influenza, is also frequently observed. In addition, pneumococcus, for which we have started to provide routine vaccination, is one of the most common bacteria that cause pneumonia. Because pneumococcal pneumonia often becomes severe, its prevention is important.
Characterized by different symptoms from those in younger people
Fever, cough, and difficulty in breathing are well-known symptoms of pneumonia. Pneumonia in elderly people is, however, characterized by different symptoms, including sudden loss of appetite, lack of energy, and sudden impairment of cognitive function (such as memory loss and an inability to perform actions that the patient used to be able to do). Although they are not apparent symptoms for pneumonia, more attention is necessary, because patients with these symptoms often have more severe pneumonia. Furthermore, the severity is not related to high fever; for example, patients with mild fever may have severe pneumonia. Even if one incidence of pneumonia is not fatal, it can trigger the further impairment of motor and cognitive functions in elderly people. If you suspect pneumonia, therefore, it is important to visit a nearby hospital and start the treatment early.
A basic treatment for pneumonia is administration of drugs called antibiotics, which kill bad bacteria. The duration of medication is 10 days to 2 weeks. For mild pneumonia, an intravenous drip at the outpatient clinic or oral drugs are used. If you need to be hospitalized, the length of stay varies depending on the severity; however, antibiotics are still used as the first treatment.
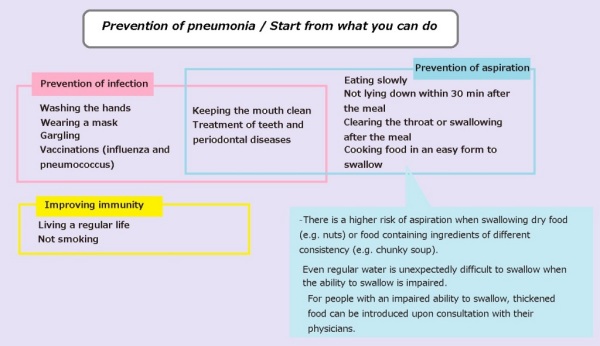
To prevent pneumonia in elderly people
To prevent aspiration pneumonia, it is important to keep the mouth clean. Dental treatment is also important, because poor condition of teeth, including periodontal diseases and many lost teeth, is more likely to increase oral bacteria and trigger aspiration. In addition, you should eat food slowly and you should not lie down within ~30 min after the meal to prevent regurgitation of digestive fluid. Clearing the throat or a swallowing after the meal is also useful, because a small amount of food may be left in the throat and it may get into the airway when the ability to swallow becomes weaker, even if you think that you swallowed everything.
To prevent pneumonia after viral infections, you should prevent viral infections by taking measures against common colds and influenza. You should wash your hands, use a mask, and gargle as your daily habit. Vaccinations are also useful for preventing pneumonia caused by influenza and pneumococcus.
Because various diseases can trigger pneumonia, more attention is required, especially if you have underlying diseases (even if these are not lung diseases or immunosuppressive diseases). Aspiration often occurs in those who had a brain infarction; they therefore have a higher risk of pneumonia.