Top > About Us > News Letter > Opening a new era of super-microsurgery
Opening a new era of super-microsurgery
Appealing to the World from the University of Tokyo Hospital
Department of Plastic, Reconstructive, and Aesthetic Surgery
Isao Koshima (Professor, Manager)
After traumatic amputation or tumor resection surgery, amputated fingers or damaged body surfaces are commonly reconstructed with grafts of skin and/or fat tissue transferred from other parts of the patient's body. For this kind of procedure, a microsurgical technique is required to perform the anastomosis of thin microvessels of around 1 mm in diameter. Our department of plastic surgery has established new surgical procedures that make use of microsurgical techniques for the performance of reconstruction after trauma or tumor resection surgery. Using current techniques, the smallest vessels that can be successfully anastomosed are generally considered to be around 1 mm in diameter. A technique enabling the anastomosis of smaller vessels would allow tissue grafting to be performed more safely and efficiently. We have been developing an anastomosis apparatus and supermicrosurgical techniques for the connection of microvessels and/or nerve fibers of around 0.3 mm of diameter using 50µ needle sutures and needles. We successfully performed the world's first supermicro anastomosis around 1990, and have since developed and publicized new surgical techniques, including the ones described below.
1. Lymphoedema
Lymphoedema is a condition of localized fluid retention and tissue swelling in the extremities that occurs after removal of the lymph nodes during resection surgery for uterine or breast cancer and can be a cause of infection, therefore disturbing the patient’s daily life. We have been developing new, innovative surgical techniques continuously since around 1990. Among them, we successfully developed a new lymphatico-venular anastomosis technique for the connection of a lymphatic vessel of 0.3 mm of diameter with a small vein under the skin in order to drain the lymph retained in the extremities into the vein. In 1996, we reported that patients with lymphedema usually present abnormalities in the smooth muscle cells of the lymphatic vessels, and suggested that lymphedema might be prevented by the performance of early stage lymphatico-venular anastomosis (prophylactic anastomosis) as quickly as possible after identification of the edema. Additionally, we also reported that the symptoms of patients with severe lymphedema preventing the lymph fluid from flowing to the heart properly could be improved by replacing the abnormal lymphatic vessels with normal vessels removed from a different part of the patient's body (functional lymph vessel transplantation) (Fig. 1).
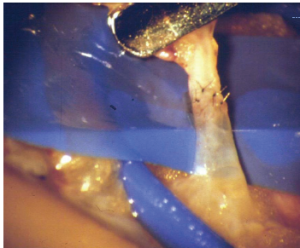
Fig. 1: Lymphatico-venular anastomosis
Becoming one of the standard surgical techniques for the treatment of lymphedema after tumor resection surgery around the world. Connecting the lymphatic vessel (clear, 0.3 mm in diameter) and the venule to reduce edema symptoms at the extremity.
2. Assessment of the lymph function with fluorescence lymphography
We previously found that the lymph fluid could not flow to the heart properly in patients with lymphedema. Therefore, we established a methodology to examine the healthy lymph system through the visualization of signals from fluorescent dyes injected subcutaneously into the tips of the lymph vessels’ extremities, using an infrared camera to trace and observe the lymphatic stream (2007). This method is becoming one of the standards for examination of the lymph system across the world.
3. Novel minimally invasive reconstruction surgery of the head and neck
Since 1989, we have been providing information about a novel thigh skin flap transplantation method to reconstruct a part of the head and neck removed in tumor resection surgery with a flap composed of skin and fat removed from the femoral area. The microsurgical technique used to connect the nutritional blood vessels contained in the flap and base, including the bone, skin flap, muscle, and other tissues, makes it possible to use different types of tissues to reconstruct the damaged area. Moreover, if a large area of the face has been damaged but at least one blood vessel remains intact, the movement control function and shape of the face can potentially be restored simultaneously using this technique (chimeric tissue transplantation). Since 2000, our tight skin flap transplantation method has become a standard reconstruction technique across the world (Fig. 2).
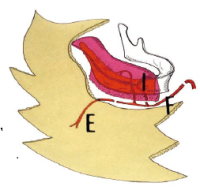
Fig. 2: Reconstruction of mandible using chimeric tissue transplantation
Reconstructing a large mandibular defect using a technique to connect the vessels contained in the skin and fat from iliac bone, thigh, and abdomen.
4. New breast reconstruction technique
In 1981, we reported a novel minimally invasive surgery technique for the reconstruction of a part or the entirety of a breast removed during tumor resection surgery with a flap including skin and fat, but no muscle, from the patient’s abdomen (transplantation of skin flap including perforators). This technique was introduced to foreign countries in 2000, and is currently one of the standard breast reconstruction techniques used around the world.
5. Applications to extremity surgery
Microsurgical techniques make it possible to replant a severed fingertip at or around the nail base, and to perform toe-to-thumb transplant surgery or a free nail bed graft to reconstruct a fingertip in the case of a deformity and/or amputation (Fig. 3). We have also reported a technique for the reconstruction of a hand or foot presenting damage to a large part of the skin or muscles using a flap comprising skin, fat, and only one nutritional blood vessel of around 0.5 mm in diameter removed from around the damaged area.
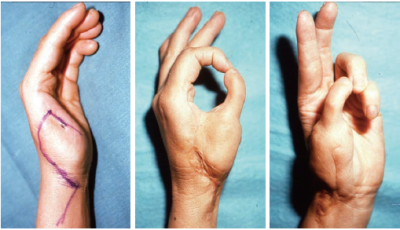
Fig. 3: Toe-to-thumb transplant surgery
Reconstructing the thumb with the second toe using a technique to connect the microvessels.
6. Live demonstration of surgery in foreign countries
Since 2000, we have been providing live demonstrations of our surgical techniques with examinations and have trained thousands of experts in 52 foreign institutions in the U.S., Belgium, ROC, Kuwait, Singapore,Spain, Holland, Russia, and others (Fig. 4).
7. Foreign visitors observing operations at our hospital
As mentioned above, we have been providing information about our reconstruction techniques involving microsurgical anastomosis to foreign nationals. Furthermore, about 500 experts from foreign institutions (including the MD Anderson Cancer Center in the U.S.) have visited the University of Tokyo Hospital to learn about our novel surgical techniques, and are now using them in their clinical practice. We hope to continue to act as a leading institution in the provision of information about newly developed microsurgical anastomosis techniques, and in demonstrating their surgical applications to domestic and international visitors.

Fig. 4: Live demonstration of surgery during training session at the State University of New York
A live demonstration of a surgery performed with techniques developed at the University of Tokyo was presented in a training session held abroad to introduce our new techniques to foreign experts.