Top > About Us > News Letter > As an original Japanese medical field, psychosomatic medicine provides appropriate medical care to contribute to society
As an original Japanese medical field, psychosomatic medicine provides appropriate medical care to contribute to society
Appealing to the World from the University of Tokyo Hospital
Department of Psychosomatic Medicine
Kazuhiro Yoshiuchi (Associate Professor, Manager)
1. What is psychosomatic medicine?
We wonder if our readers are acquainted with psychosomatic medicine. While they have probably heard of it, they may not quite understand this medical field and the difference between psychosomatic medicine and psychiatry.
Psychosomatic medicine can be defined as a field of internal medicine that uses psychotherapy concomitantly to treat diseases. This field was established as a subspecialty of internal medicine for the treatment of stress-related physical diseases, called psychosomatic diseases (e.g., lifestyle-related diseases, headache, irritable bowel syndrome, etc.). In Japan, the first department of psychosomatic medicine was established at the Kyushu University School of Medicine in 1963. Subsequently, another department was opened at the University of Tokyo in 1972. Psychosomatic medicine is a unique medical field that only exists in Japan and Germany.

Fig. 1: Staff members of the Department of Psychosomatic Medicine
2. Treatments provided by the Department of Psychosomatic Medicine of the University of Tokyo Hospital
We focus on the treatment of eating disorders and of the aforementioned stress-related psychosomatic diseases. Moreover, we also provide psychological care for patients who suffer from various physical diseases, including cancer. The medical field that provides psychological care to cancer patients is called psycho-oncology. A physician specializing in psychosomatic medicine treats cancer patients as a member of the palliative care team. In addition, physicians affiliated to the Department of Psychosomatic Medicine have been providing psychological support to all patients receiving hematopoietic stem cell transplantation from the Department of Hematology and Oncology since 1996. To date, we have supported approximately 500 patients. The basic concept shared by these medical approaches is the idea – characteristic of psychosomatic medicine – that attention should be paid not only to the disease, but also to the patient as a full human being, as well as to the patient’s family and environment. By taking this whole-patient approach, we promote holistic medicine.
3. Outpatient care
Although the number of staff members is limited, we treat new patients every day. Besides these new patients, many more are referred to this department by other departments of the hospital. To cope with these specific circumstances, we classify patients into different categories of in-hospital referrals. The many patients with eating disorders who present to this department are categorized as eating disorder patients. Patients can also be referred to this department by external hospitals. The latter are categorized as community healthcare collaboration patients. This category comprises three subcategories: general referrals, referrals requiring treatment for eating disorders, and referrals requiring psycho-oncological treatment. In this way, we have been accepting an increasing number of referrals from external hospitals.
4. Inpatient care
Physicians specialized in psychosomatic medicine form a team to provide medical treatment in the internal medicine ward. Currently, there are only a small number of inpatient facilities for patients suffering from eating disorders in Japan. To improve this situation, we accept more patients suffering from physically serious anorexia nervosa, and provide them with inpatient treatment. The aforementioned team provides appropriate medical treatment to individual inpatients. All staff members of the Department of Psychosomatic Medicine get together in a weekly conference to discuss the conditions of inpatients. After this discussion, all of the staff members, including the department manager, do a round.
5. Research
We have been involved in projects to develop psychological tests. Thus, we developed the Tokyo University Egogram New Ver. II (TEG New Ver. II), the character analysis tool most frequently used in Japan. This egogram has been widely used not only in the healthcare field, but also in the industrial and educational fields. Although we examine patients carefully and conduct detailed tests at the hospital, we also need to observe and assess the patients in their daily lives in order to clarify the relationship between stress and diseases precisely. Due to the lack of effective assessment methods, the patient’s daily life has been regarded as something like a black box that we cannot access. For more than 15 years, we have been engaged in a project to develop a portable or wearable computer (or more recently, a smartphone application) to record the patient’s daily life conditions. Using this ecological momentary assessment, we have been recording patients’ daily life conditions and have attempted to clarify the pathological conditions of various stress-related diseases. In this process, we have promoted the development of a software to record meals with absolute accuracy in collaboration with the Department of Diabetes and Metabolic Diseases of the University of Tokyo Hospital. Last year, we partially succeeded in predicting patients’ mood states according to their accelerometer data, and published promising results ahead of concurrent researchers from other countries.
Fig. 2: TEG New Ver. II developed by the Department of Psychosomatic Medicine
6. Future trend
In the healthcare field, stress and psychological problems are treated with less objectivity, which still results in lack of evidence. Our department has progressively introduced state-of-the-art technologies, including wearable information devices, to develop new diagnostic and treatment methods and to generate evidence in the field of psychosomatic medicine. Through this approach, we aim to provide patients with better medical care.

Fig. 3: Wearable computer-based data collector for daily life
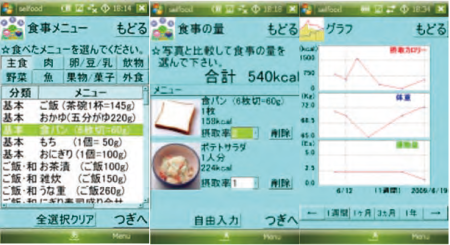
Fig. 4: Software for meal recording developed by the Department of Psychosomatic Medicine and the Department of Diabetes and Metabolic Diseases