Top > About Us > News Letter > Department of Urology leads the world in the research of intractable diseases and its clinical application
Department of Urology leads the world in the research of intractable diseases and its clinical application
Message from the University of Tokyo Hospital to the World
Department of Urology and Andrology, Professor and Chairman, Yukio Homma, M.D. & Ph.D.
(1) Approaches in the Department of Urology
At the Department of Urology, we provide surgical and non-surgical treatment of diseases in the kidneys, the ureters, the urinary bladder, the prostate, the testes, and the male reproductive organ. Nineteen full-time doctors, including Professor Homma, provide medical treatments to ~28,000 outpatients and ~1,200 inpatients, as well as perform ~1,000 operations every year. We provide evidence-based, high-quality medical service, while also working on two major projects, which are the development and research of “treatment of intractable diseases” that cannot be treated in any other hospitals and “novel surgical procedures”.
(2) Treatment of intractable diseases
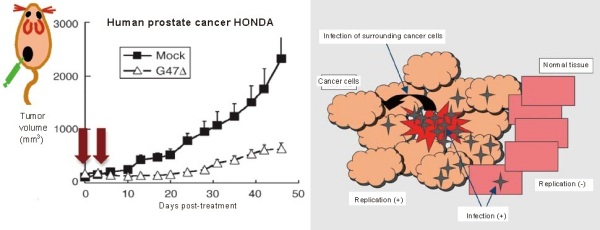
Fig. 1. Virus therapy against prostate cancer
2-1. Virus therapy against treatment-resistant prostate cancer
A representative intractable disease is cancer that is resistant (not responsive) to treatment. In the field of urology, the typical example is a prostate cancer that has become resistant to hormone therapy. Whereas new anti-cancer drugs or androgen antagonists have been under development, we have been applying a treatment with novel viruses in a clinical setting. The virus used is G47 (delta), in which triple mutations were introduced into herpes simplex virus type I.
Once a herpes virus infects a host cell, viral replication occurs leading to cell death (a cytotoxic effect). Mutations of the viral genes enable the virus to replicate in a cancer cell but not in a normal cell. Therefore only cancer cells are specifically killed during the process of viral replication. Replicated viruses spread out and infect other cancer cells; as a result, this cycle produces an anti-tumor effect, whereas there is no effect on normal cells (Fig. 1).
In our experiments, the subcutaneous transplantation of treatment-resistant human prostate cancer cells in mice resulted in the rapid proliferation of the cancer cells; however, this was inhibited by administration of G47 viruses (Fig. 1). Because its efficacy was experimentally proved and its safety was confirmed in human, this viral therapy is currently under investigation in a phase I clinical trial in our hospital. We already observed some responders and we expect that this therapy will be used as an actual treatment in the near future.
In addition, we have been working on the treatment of intractable cancer using dendritic cells and peptide vaccines.
2-2. Treatment and investigation of the pathogenesis of interstitial cystitis
Interstitial cystitis is not fatal, but is important as an intractable urological disease. This disease has a significant impact on the patient’s life because of the symptoms, such as frequent urination, urinary urgency (a strong need to urinate), and bladder pain; however, its cause and effective treatment are unknown.
In our department, we have actively engaged in the medical care of interstitial cystitis, and we have been achieving favorable outcomes with various treatments, such as bladder hydrodistention, botulinum toxin injection into the bladder wall, and intravesical instillation with heparin and lidocaine. Because we also engage in educational activities, including consultation meetings with patients, we have the largest number of patients with interstitial cystitis in Japan.
With regard to research, we pointed out that endoscopic findings of interstitial cystitis are categorized into two subtypes (Fig. 2). We also showed in collaboration with the Department of Pathology that these two subtypes also have completely different pathological features. Analyzing the molecular characterization of bladder tissues indicates that the expression of receptors for noxious stimuli (stimuli that damage tissues) is increased, and that leukocytes that infiltrate the bladder may produce a specific type of antibody in the bladders of patients with interstitial cystitis. From these findings, we are coming close to elucidating the pathogenesis that is so far unknown.

Fig. 2. Cytoscopic findings of interstitial cystitis depending on the disease subtypes
a. Normal bladder
No abnormal vessels or hemorrhage are observed
b. Hunner type interstitial cystitis
Aggregated abnormal vessels (Hunner’s lesions) are observed
c. Non-Hunner type interstitial cystitis
Punctate hemorrhage is extensively observed after bladder hydrodistention
(3) Novel surgical procedures
Of all of the development of surgical procedures that have been achieved over time, robot-assisted surgery can be a revolutionary step. In terms of procedures, this is considered to be a developed form of laparoscopic surgery; however, this robot-assisted surgery brings an expanded 3-D view using a robotic arm with more dexterity and mobility than the human hand as an innovative technology. Once you see the actual robot-assisted surgery, you will realize that it is on a different level compared to conventional laparotomy.
In the last three years, almost all cases of radical prostatectomy for prostate cancer patients that were performed in our department were robot-assisted. Robot-assisted surgery provides favorable postoperative outcomes and especially improves urinary incontinence, which frequently occurs after radical prostatectomy, at the early stage. To improve these outcomes, it is important to cooperate with nursing staff as well as master the robotic arm (Fig. 3).
In addition to radical prostatectomy, total cystectomy for bladder cancer and partial nephrectomy for renal carcinoma are performed by robot-assisted surgery as advanced medical treatments. Robot-assisted surgery has also been applied to other fields. When we look back from the future on the current times, this procedure will be evaluated as a technology that has changed surgical medicine entirely.
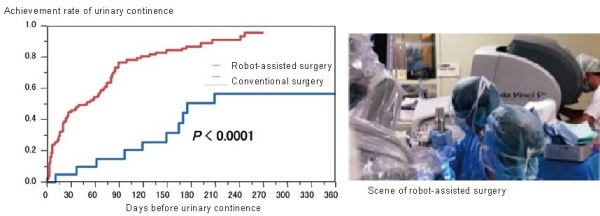
Urinary continence is achieved earlier after robot-assisted surgery than after conventional surgery.
Fig. 3. Achievement rate of urinary continence