
Mutsumi Okazaki, M.D., Ph.D.
Professor and Chair, Department of Plastic and Reconstructive Surgery,
Graduate School of Medicine, The University of Tokyo.
【Profile】
1990 Graduated from The University of Tokyo, School of Medicine.【Field of expertise】
・Reconstruction of facial deformity and dysfunction【Reanimation of Facial Paralysis】
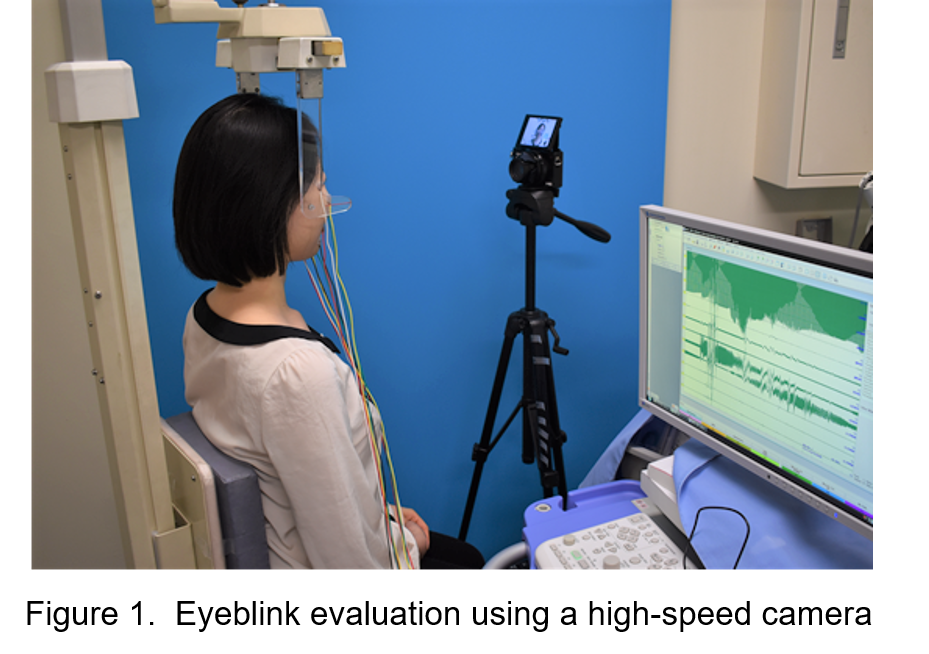
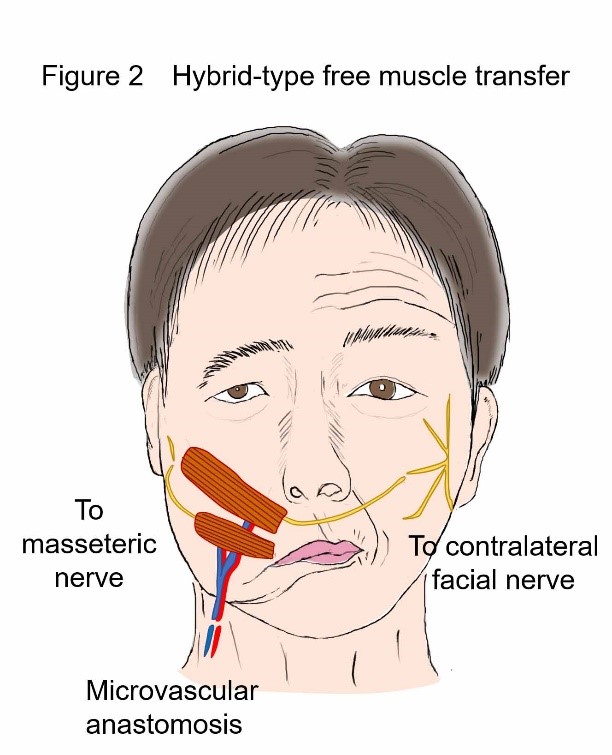
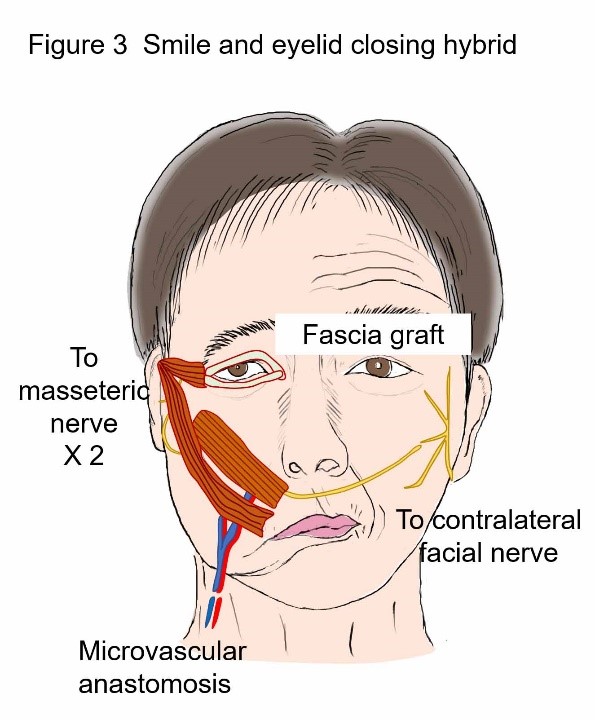
At Plastic and Reconstructive Surgery in The University of Tokyo Hospital, we perform surgical operations that are highly satisfying for patients using our ideas and ingenious and dexterous techniques, and had published the achievements obtained for the benefit of the world. Here we present our surgical treatments of facial nerve paralysis| However, symptoms that trouble patients are related to eyeblink, such as corneal inflammation and dryness or pain in the eyes. Therefore, in 2016, our division introduced an eyeblink evaluation using a high-speed camera. An eyeblink test is conducted on patients with facial nerve paralysis, with several tens of thousands of frames analyzed with each test. Based on the analysis results, a reconstructive procedure for the area around the eyes that best suits each patient is determined, as well as the appropriate amount of correction (Figure 1). |
 |
 |  |
| 3. More complex reconstruction of facial features and functional disorders Major deformation of the face may result in patients with bone or soft tissue defects in addition to facial nerve paralysis, due to tumor resection or traumatic injury. For such patients, we perform surgery to transplant vascularized bones and adipose tissue at the same time as muscle (Figure 4). Simultaneous implementation of such a complex procedure reduces the required number of surgical operation sessions, thereby relieving burden to the patient, and also supporting faster rehabilitation. | 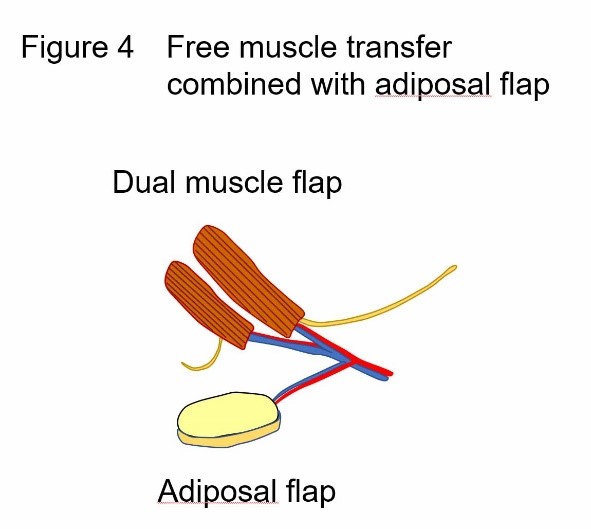 |
1. Okazaki M, Tanaka K, Uemura N, Usami S, Homma T, Okubo A, Hamanaga M, Mori H. One-Stage Dual Latissimus Dorsi Muscle Flap Transfer with a Pair of Vascular Anastomoses and Double Nerve Suturing for Long-Standing Facial Paralysis. J Plast Reconstr Aesthet Surg. 2015; 68: e113-9.
2. Homma T, Okazaki M, Tanaka K, Uemura N. Simultaneous Surgical Treatment for Smile Dysfunction and Lagophthalmos Involving a Dual Latissimus Dorsi Flap. Plast Reconstr Surg Glob Open. 25; 5: e1370, 2017.
【Selected Publications】
・Hidaka T, Kurita M, Ogawa K, Tomioka Y, Okazaki M. Application of Artificial Intelligence for Real-time Facial Asymmetry Analysis. Plast Reconstr Surg. 2020 (Online ahead of print).
・Mito D, Kurita M, Miyamoto S, Okazaki M. Miniaturization of Indocyanine Green Fluorescence Imaging Device Using a Smartphone.Plast Reconstr Surg. 145:230e-232e, 2020.
・Higashino T, Okazaki M, Mori H, Yamaguchi K, Akita K. Microanatomy of Sensory Nerves in the Upper Eyelid: A Cadaveric Anatomical Study. Plast Reconstr Surg. 142: 345-353, 2018.
・Tanaka K, Yano T, Homma T, Tsunoda A, Aoyagi M, Kishimoto S, Okazaki M. A new method for selecting auricle positions in skull base reconstruction for temporal bone cancer. Laryngoscope. 2018 [Epub ahead of print].
・Usami S, Okazaki M. Fingertip reconstruction with a posterior interosseous artery perforator flap: A minimally invasive procedure for donor and recipient sites. J Plast Reconstr Aesthet Surg. 2017; 70: 166-172.
・Homma T, Okazaki M, Tanaka K, Uemura N. Simultaneous Surgical Treatment for Smile Dysfunction and Lagophthalmos Involving a Dual Latissimus Dorsi Flap. Plast Reconstr Surg Glob Open. 25; 5: e1370, 2017.
・Okazaki M. Aging and Melanocytes Stimulating Cytokine Expressed by Keratinocyte and Fibroblast. Textbook of Aging Skin, Second Edition, Miranda A. Farage, Kenneth W. Miller and Howard I. Maibach eds. Springer Berlin Heidelberg, 415-422, 2016.
・Uemura N, Okazaki M, Mori H. Anatomical and histological study to determine the border of sole skin Surg Radiol Anat. 2016;38:767-73.
・Okazaki M, Tanaka K, Uemura N, Usami S, Homma T, Okubo A, Hamanaga M, Mori H. One-Stage Dual Latissimus Dorsi Muscle Flap Transfer with a Pair of Vascular Anastomoses and Double Nerve Suturing for Long-Standing Facial Paralysis. J Plast Reconstr Aesthet Surg. 2015; 68:e113-9.
・Mori H, Uemura N, Okazaki M. Nipple reconstruction with banked costal cartilage after vertical-type skin-sparing mastectomy and deep inferior epigastric artery perforator flap. Breast Cancer 2015; 22: 95-97.
・Wakimura Y, Wang W, Itoh S, Okazaki M, Takakuda K. An experimental study to bridge a nerve gap with a decellularized allogeneic nerve. Plast Reconstr Surg. 2015; 136: 319e-27e.
・Tanaka K, Okazaki M, Yano T, Miyashita H, Homma T, Tomita M. Quantitative evaluation of blood perfusion to nerves included in the anterolateral thigh flap using indocyanine green fluorescence angiography: a different contrast pattern between the vastus lateralis motor nerve and femoral cutaneous nerve. J Reconstr Microsurg. 2015; 31: 163-70.
・Tanaka K, Okazaki M, Yano T, Akiyama M, Mori H. Volumetric changes in transplanted vascularized fat flaps after ischemic or congestive stresses and their relationship to capillary density in a Zucker fatty rat model. Microsurg. 2015; 35: 653-61.
・Yano T, Okazaki M, Yamaguchi K, Akita K. Anatomy of the middle temporal vein: implications for skull-base and craniofacial reconstruction using free flaps. Plast Reconstr Surg. 2014; 134: 92e-101e.
・Okazaki M. Functional and esthetic reconstruction of the defects following the hemiglossectomy in patients with oropharyngeal cancer. Head and Neck Cancer (ISBN978-953-51-0236-6) Mark Agulnik ed., pp337-348 INTEC, Croatia, 2012.
・Yano T, Okazaki M, Tanaka K, Iida H, Aoyagi M, Kishimoto S. A new concept for classifying skull-base defects for reconstructive surgery. J Neurol Surg B Skull Base. 2012; 73: 125-31.
・Kurita M, Okazaki M, Kaminishi-Tanikawa A, Niikura M, Takushima A, Harii K. Differential expression of wound fibrotic factors between facial and trunk dermal fibroblasts. Connect Tissue Res 2012; 53: 349-54.
・Okazaki M, Miyamoto S. Low skin paddle pedicled latissimus dorsi flap with vascular supercharging: Possibility of complete survival of larger and/or more distal flap. Plast Reconstr Surg, 2011; 128 : 568e-9e
・Kurita M, Okazaki M, Fujino T, Takushima A, Harii K. Cyclic stretch induces upregulation of endothelin-1 with keratinocytes in vitro: Possible role in mechanical stress-induced hyperpigmentation. Biochem Biophys Res Commun. 2011; 409: 103-7.
・Kurita M, Okazaki M, Ozaki M, Tanaka Y, Tsuji N, Takushima A, Harii K. Patient satisfaction after open reduction and internal fixation of zygomatic bone fractures. J Craniofac Surg. 2010; 21: 45-49.
・Okazaki M, Ueda K, Sasaki K, Shiraishi T, Kurita M, Harii K. Expanded narrow subcutaneous-pedicled island forehead flap for reconstruction of the forehead. Ann Plast Surg, 2009; 63: 167-70.
・Takushima A, Harii K, Okazaki M, Ohura N, Asato H. Availability of latissimus dorsi minigraft in smile reconstruction for incomplete facial paralysis: quantitative assessment based on the optical flow method. Plast Reconstr Surg. 2009; 123: 1198-208.
・Okazaki M, Asato H, Okochi M, Suga H, Kinoshita M. Shortcut vascular augmented long rectus abdominis musculocutaneous flap transfer using intercostal perforator for complex oro-pharyngo-cutaneous defects. Plast Reconstr Surg, 2008; 121: 220e-221e.
・Miyamoto S, Okazaki M, Ohura N, Shiraishi T, Takushima A, Harii K. Comparative study of different combinations of microvascular anastomoses in a rat model: end-to-end, end-to-side, and flow-through anastomosis. Plast Reconstr Surg, 2008; 122: 449-55.
・Miyamoto S, Okazaki M, Takushima A, Shiraishi T, Omori M, Harii K. Versatility of a posterior-wall-first anastomotic technique using a short-thread double-needle microsuture for atherosclerotic arterial anastomosis. Microsurg. 2008; 28: 505-8.
・Okazaki M, Asato H, Takushima A, Sarukawa S, Nakatsuka T, Yamada A, Harii K. Analysis of salvage treatments following failure of the free flap transfer due to vascular thrombosis in reconstruction for head and neck cancer. Plast Reconstr Surg, 2007; 119: 1223-1232.
・Okazaki M, Asato H, Takushima A, Sarukawa S, Okochi M, Harii K. Reconstruction with rectus abdominis myocutaneous flap for total glossectomy with laryngectomy. J Reconstr Microsurgery 2007; 23: 243-249.
・Okazaki M, Asato H, Okochi M, Suga H. One-segment double vascular pedicled free jejunum transfer for the reconstruction of pharyngoesophageal defects. J Reconstr Microsurgery 2007; 23: 213-218.
・Ueda K, Kajikawa A, Suzuki Y, Okazaki M, Nakagawa M, Iida S. Blood gas analysis of the jejunum in the supercharge technique: to what degree does circulation improve? Plast Reconstr Surg. 2007; 119:1745-50.
・Okazaki M, Asato H, Takushima A, Nakatsuka T, Sarukawa S, Inoue K, Harii K, Sugawara Y, Makuuchi M. Hepatic artery reconstruction with double-needle micro-suture in living donor liver transplantation. Liver Transpl, 2006; 12: 46-50.
・Takushima A, Harii K, Asato H, Momosawa A, Okazaki M. One-stage reconstruction of facial paralysis associated with skin/soft tissue defects using latissimus dorsi compound flap. J Plast Reconstr Aesthetic Surg 2006; 59: 465-473.
・Hasegawa H, Okazaki M, Sasaki K. Restoration of the thumb abduction damaged by electrical burn using free dorsalis pedis flap with the extensor hallucis brevis tendon. J Reconstr Microsurgery 2006; 22: 33-36.
・Okazaki M, Asato H, Sarukawa S, Takushima A, Nakatsuka T, Harii K. Availability of end-to-side arterial anastomosis to the external carotid artery using short-thread double-needle micro-suture in free-flap transfer for head and neck reconstruction. Ann Plast Surg, 2006; 56: 171-175.
・Okazaki M, Hasegawa H, Kano M, Kurashina R. A different method of fingertip reconstruction with the thenar flap. Plast Reconstr Surg 2005; 115: 885-888.
・Okazaki M, Asato H, Takushima A, Nakatsuka T, Ueda K, Harii K. Secondary reconstruction of failed esophageal reconstruction. Ann Plast Surg 2005; 54: 530-537.
・Okazaki M, Yoshimura K, Uchida G, Harii K. Correlation between age and the secretions of melanocyte-stimulating cytokines in cultured keratinocytes and fibroblasts. Br J Dermatol 2005; 153 (s3): 23-29.
・Okazaki M, Asato H, Sarukawa S, Okochi M. A revised method for pharyngeal reconstruction using free jejunal transfer. Ann Plast Surg 2005; 55: 643-647.
・Okazaki M, Yoshimura K, Fujiwara H, Suzuki Y, Harii K. Induction of hard keratin in non-nail-matrical keratinocytes by nail-matrical fibroblasts through epithelial-mesenchymal interaction. Plast Reconstr Surg 2003; 111: 286-290.
・Okazaki M, Yoshimura K, Suzuki Y, Uchida G, Kitano Y, Harii K, Imokawa G. Epidermal hyperpigmentation mechanisms in Café-au-lait macules of Neurofibromatosis type-I (von Recklinghausen’s disease) may be associated with dermal fibroblast-derived stem cell factor and hepatocyte growth factor. Br J Dermatol 2003; 148: 689-697.
・Okazaki M, Ohmori K, Akizuki T. Long-term follow-up of nasomaxillary epithelial inlay skin graft for the saddle nose. Plast Reconstr Surg 2003; 112: 64-70.
・Okazaki M, Yoshimura K, Suzuki S, Harii K. Effects of subepithelial fibroblasts on epithelial differentiation in human skin and oral mucosa: Heterotypically recombined organotypic culture model. Plast Reconstr Surg 2003; 112: 784-792.
・Okazaki M, Yoshimura K, Uchida G, Harii K. Elevated expression of Hepatocyte and Keratinocyte Growth Factor in cultured buccal-mucosa-derived fibroblasts compared with normal-skin-derived fibroblasts. J Dermatol Sci 2002; 30: 108-115.
・Okazaki M, Ueda K, Niu A, Momosawa A. Free lateral supramalleolar flap transfer as a small and thin flap. Ann Plast Surg 2002; 49: 133-137.
・Okazaki M, Akizuki T, Ohmori K. Medial canthoplasty with Mitek Anchor System. Ann Plast Surg 1997; 38: 124-128.